Leptospirosis: What You Need to Know
Imagine taking a cool swim in a freshwater lake on a hot summer day, volunteering to clean up your community after a flood, or nursing your beloved family dog back to health. These common scenarios feel worlds apart, yet they are all linked by a hidden threat: a widespread but frequently overlooked bacterial disease called leptospirosis.
Caused by corkscrew-shaped bacteria of the genus Leptospira, this infection is a zoonosis, meaning it is transmitted from animals to humans, typically through contact with water or soil contaminated by animal urine. Because its symptoms are so varied and non-specific, it is often misdiagnosed, underreported, and misunderstood. The implications of this hidden disease are profound, affecting everything from public health responses to our relationship with the environment and even our pets.
This article pulls back the curtain on one of the world's most common zoonotic diseases. Here are five of the most surprising and counter-intuitive truths about leptospirosis that reveal its complex nature and highlight the importance of awareness.
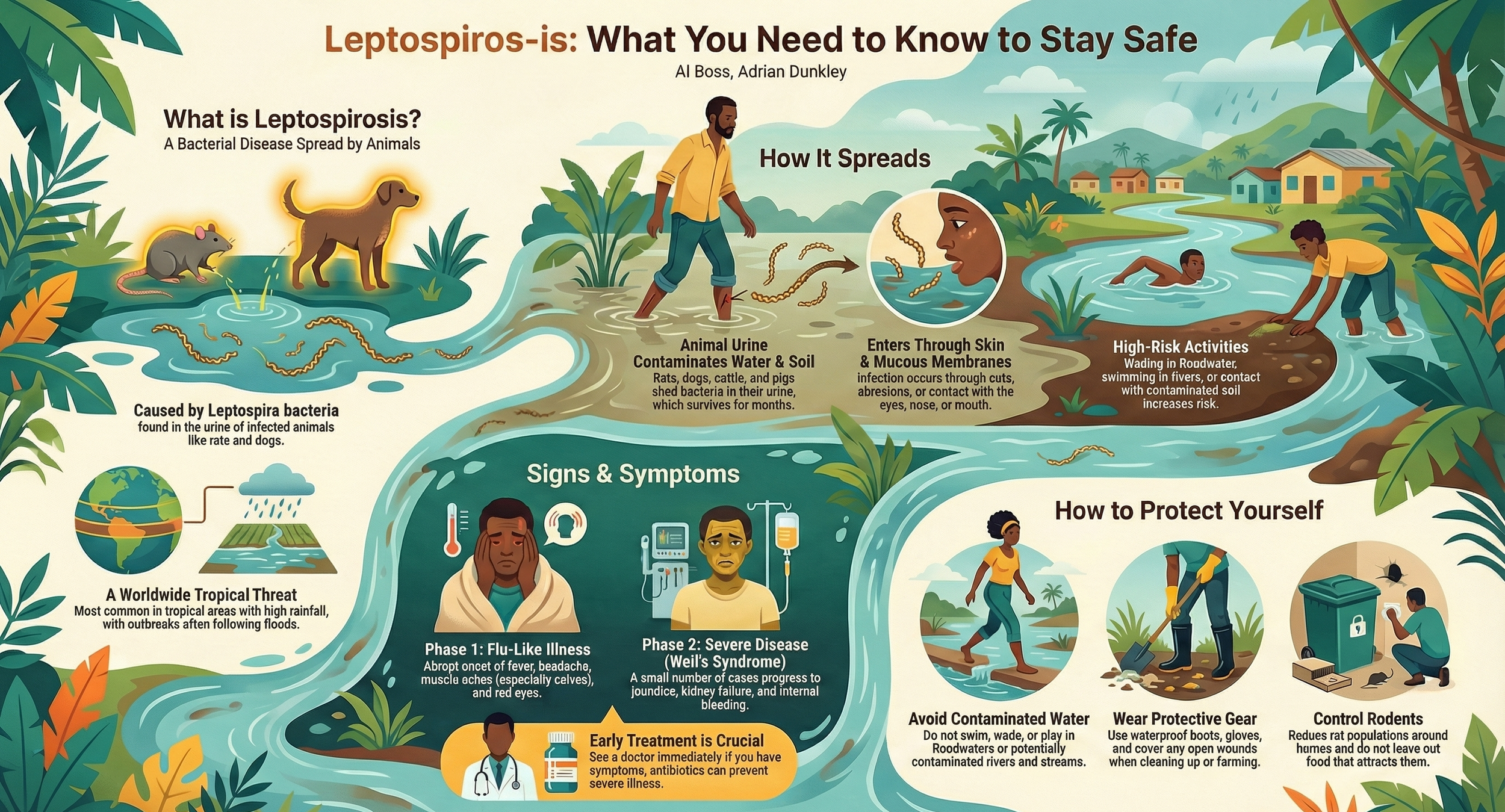
Infographic of Leptospirosis: What You Need to Know
1. It's a Master of Disguise, Often Mistaken for the Flu or Dengue.
One of the greatest challenges in identifying leptospirosis is that its initial presentation is notoriously vague. The disease often begins with an abrupt onset of non-specific symptoms, including fever, headache, muscle aches (myalgia), chills, and red eyes (conjunctival suffusion). These symptoms can easily be mistaken for a wide range of more common illnesses.
According to the World Health Organization (WHO), leptospirosis is a great mimic, presenting like influenza, dengue, meningitis, and hepatitis. This mimicry is especially dangerous in tropical regions where it can be misdiagnosed as dengue fever. The clinical overlap can be deadly; while the management of dengue is symptomatic, leptospirosis is a bacterial infection that is treatable with antibiotics. To make matters even more complicated, the two can occur as a coinfection, presenting a profound diagnostic challenge for clinicians. As one case study notes, "The comparable clinical symptoms of both infections make it challenging to distinguish between leptospirosis and dengue." An accurate and timely diagnosis is therefore critical to ensure patients receive the correct care.
The diagnostic difficulty is a core feature of the disease, as emphasized by the WHO:
"Leptospirosis may present with a wide variety of clinical manifestations. These may range from a mild “flu”-like illness to a serious and sometimes fatal disease. It may also mimic many other diseases, e.g. dengue fever and other viral haemorrhagic diseases."
2. Your Pet's Role in Transmission Is More Complicated Than You Think.
While rodents are recognized as the most important reservoirs for leptospirosis, many people know that domestic animals, including dogs, can also carry and transmit the bacteria. What's surprising, however, is that the risk isn't as straightforward as it seems. A large systematic review found that studies assessing contact with dogs or cats showed a median odds ratio "close to unity," indicating that in many settings, routine pet contact is not a major statistical risk factor for infection.
However, this statistical trend should not be mistaken for a lack of risk. The danger lies in specific circumstances where pets can become significant sources of transmission. A powerful real-world example occurred in Nicaragua following an epidemic after heavy flooding. Researchers found that "the epidemic likely resulted from exposure to flood water which was contaminated by urine from infected dogs," demonstrating that under the right environmental conditions, our canine companions can become a major vector.
Adding another layer of complexity is the role of vaccination. Pet owners may feel secure knowing their dog is vaccinated, but this protection isn't absolute. While immunization protects an animal against the disease, research shows it "does not completely abolish the carrier state, allowing for continued excretion." But the nuance goes even deeper: "several outbreaks associated with immunised dogs have been reported. These are usually caused by serovars which have been previously rarely reported in dogs, so the antigens are not included in the canine vaccines." In other words, even a vaccinated dog can shed bacteria, sometimes of a strain the vaccine doesn't even cover, posing a hidden risk to its human family.
3. Summer Fun and Natural Disasters Share a Common Threat: Water.
The primary route of leptospirosis transmission is environmental. The bacteria are shed in the urine of infected animals and can survive for weeks to months in contaminated water or moist soil. This single fact creates two very different patterns of risk around the globe, turning both idyllic summer pastimes and catastrophic events into potential sources of infection.
A systematic review of transmission determinants identified these distinct scenarios:
• In developed countries, such as those in North America and Europe, the risk is most often linked to "recreational exposure." Activities like swimming, kayaking, canoeing, and participating in triathlon events can bring people into contact with contaminated freshwater sources.
• In resource-poor countries, particularly on islands and in Asia, "floods and heavy rain" are among the most significant drivers of large-scale outbreaks.
This link between natural disasters and disease is starkly illustrated by real-world events. Following a hurricane, one news report noted that Jamaica experienced an outbreak because "the passage of Hurricane Melissa which has created conditions that have increased the risk of exposure to contaminated water and soil." The same water that fuels our summer fun can, under different circumstances, become a widespread public health threat.
4. Recovery Isn't Always the End of the Story.
For most patients, leptospirosis is an acute illness from which they completely recover. However, for a subset of individuals, the infection can leave a lasting impact in the form of late sequelae—long-term health issues that persist after the initial sickness has passed. The feeling of being "better" doesn't always mean the bacteria is gone for good.
The WHO guidance documents a range of neuropsychiatric symptoms that can follow the acute phase, including "chronic fatigue," as well as "headache, paresis, paralysis, mood swings and depression." The mechanism behind many of these is not fully understood, but one of the most unique long-term effects is related to the eyes.
After the immune system clears the bacteria from the blood and most organs, leptospires "may persist in the eyes for much longer." Because the eyes are an "immunologically privileged site," the bacteria can be "sheltered from the patient's immune response." This persistence can lead to ocular symptoms like uveitis and iridocyclitis (inflammation of different parts of the eye) as a late presentation of the disease, sometimes occurring months or even years after the initial infection, serving as a debilitating reminder of the bacteria's resilience.
5. We Know How to Fight It: Controlling Rodents Works.
While the disease is complex and adaptable, leptospirosis is not an insurmountable public health challenge. There are proven, high-impact interventions that can dramatically reduce its prevalence, centering on the primary source of transmission.
Rodents are consistently recognized as the "most important and widely distributed reservoirs of leptospiral infection." This makes rodent control a powerful tool. A compelling success story comes from Gujarat, India, where several districts were endemic for the disease. After organizing large-scale, community-based rodent control campaigns in 1,822 villages, health officials documented an impressive 83% reduction in the disease prevalence.
This remarkable outcome demonstrates that coordinated public health efforts targeting the main animal reservoir can be highly effective. By reducing the rodent population, the amount of bacteria shed into the environment is also reduced, breaking the chain of transmission and protecting human populations. It's a clear reminder that understanding the source is the key to prevention.
Conclusion
Leptospirosis is far more than a simple "rat fever." It is a complex, adaptable zoonotic disease that mimics other illnesses, complicates our relationship with pets, and thrives in environments ranging from recreational lakes to disaster zones. Its ability to persist in the body long after recovery further underscores its insidious nature.
Yet, despite its ability to hide in plain sight, it is a disease we know how to combat through targeted public health strategies. The success of rodent control campaigns proves that understanding and interrupting its transmission cycle can save lives. This leaves us with a final, sobering question: Given its ability to mimic common illnesses and spread through our environment in unexpected ways, how many cases of 'the flu' each year might actually be something else entirely?